The Next-Generation Prior Authorization Solution

Our Mission
To create a more efficient healthcare system and eliminate waste by streamlining prior authorization and utilization management.
A new approach for payers and providers
Healthcare has a waste waste
waste waste waste waste problem
A big part of that problem? Prior authorization processing – a $31B challenge for the healthcare industry. It also accounts for more than 30% of all preventable write-offs for hospitals and providers.
That’s because hospitals and clinics commit a tremendous amount of time, staff, and resources to an inefficient approval process. Physicians spend nearly an hour per day on prior authorizations, while staff members spend an additional 19 hours per week dealing with payer approvals. It’s no surprise why prior authorizations are the number one cause of provider burnout.
The whole process requires hours of manual reviews, creates additional paperwork, and strains workflow efficiency. All of this inefficiency drains cash for both providers and payers. Providers spend nearly $11 per transaction to conduct a prior auth manually and nearly $4 using a web portal.
In a world where only 13% of prior authorizations are processed electronically, it’s a lot of waste.
Prior Authorization
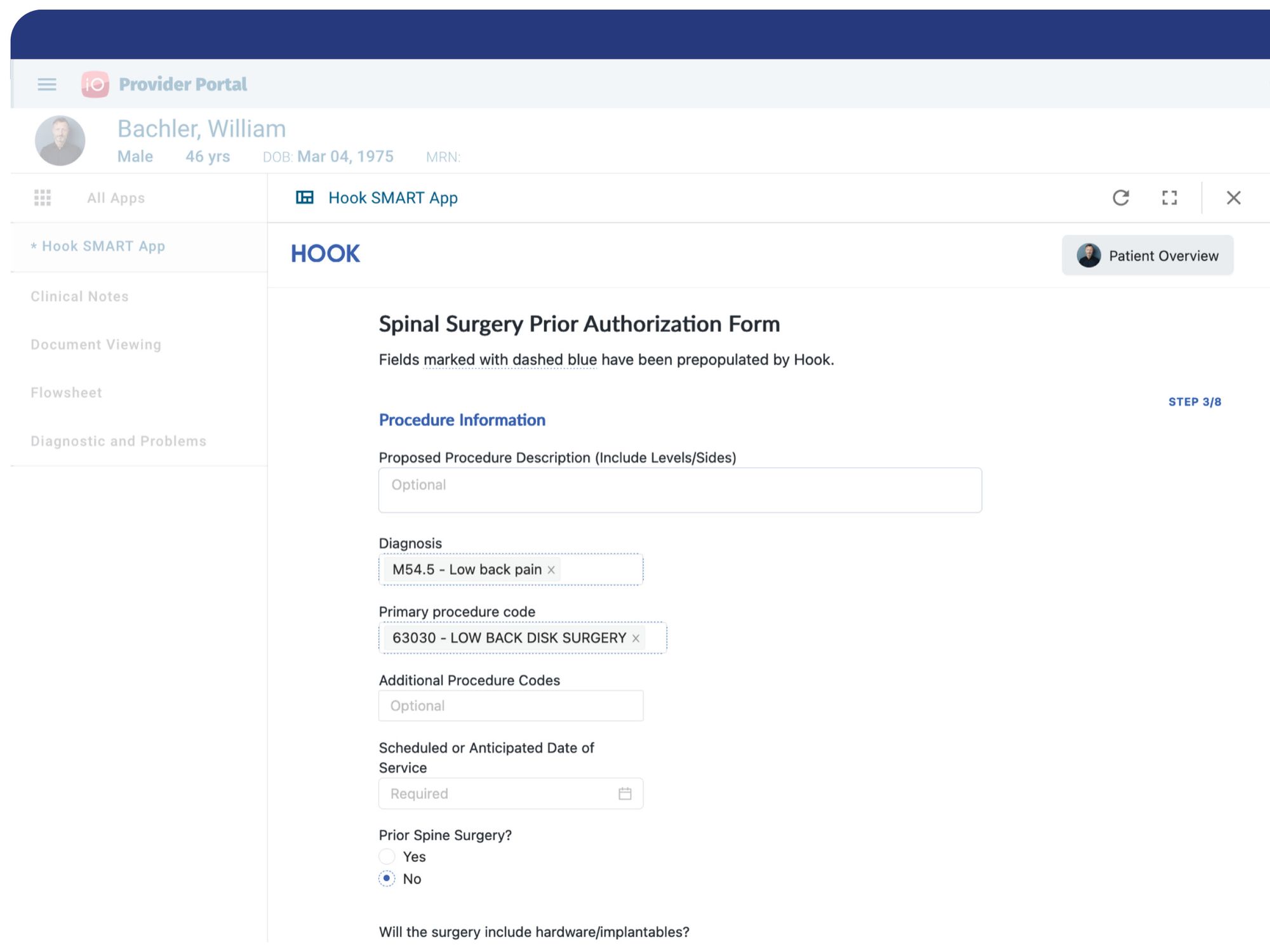
Hook streamlines the entire end-to-end prior authorization process, eliminating outdated paperwork, manual review processes, and workflow inefficiency. Using CDS Hooks, CQL and SMART on FHIR, prior auths are automated and transactions happen in seconds.